Aerophagia: Symptoms, Treatment, and Relief for CPAP Users and Sleep Apnea
If you make use of a CPAP machine to treat your obstructive sleep apnea, you may have found yourself experiencing an increase in intestinal gas, bloating, or belching. Aerophagia, a usually harmless but common side effect of CPAP treatment may be what you’re experiencing. In this article, we’ll discuss the common symptoms, causes, and treatment of Aerophagia.
What is Aerophagia?
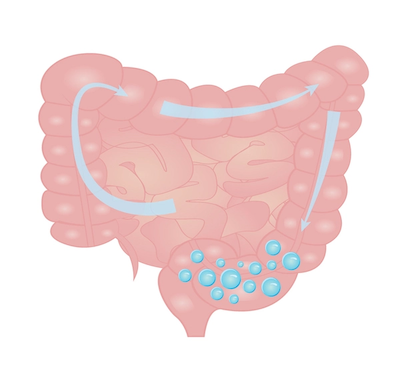
People constantly and naturally take in air whenever we eat or talk. When we have air in our system, it usually expels itself through a burp or works its way through our systems as flatulence. However, some people are unknowingly swallowing air, more than is common, resulting in a medical condition known as aerophagia (from the Greek, meaning to eat air). Although Aerophagia is usually harmless, it can cause some discomfort to those experiencing it, particularly in the gastrointestinal system.
For people using CPAP machines, aerophagia can occur because of the constant air pressure keeping airwaves open throughout the night, resulting in more air being taken into the body.
Aerophagia can often indicate the presence of other disorders inside the gastroesophogael system, or in some cases, psychological disorders such as anxiety and panic attacks.
Aerophagia Symptoms
Aerophagia has symptoms that are common in other gastrointestinal illnesses, such as gastroesophageal reflux disease (GERD) and irritable bowel syndrome, which can make it difficult to diagnose. These include:
Frequent belching: One of the hallmark symptoms of aerophagia is excessive belching or reflux. If you find yourself burping more frequently than usual, it could be a sign of excessive air in your digestive system.
Abdominal bloating: Aerophagia often leads to bloating, causing discomfort and a feeling of fullness in the abdomen. This bloating may be accompanied by visible distension or tightness in the stomach area.
Flatulence: Excess swallowed air can result in increased gas production, leading to increased flatulence. This can be embarrassing and uncomfortable for those experiencing aerophagia.
Abdominal pain or cramps: Some individuals with aerophagia may experience abdominal pain or cramps due to the excessive air in their digestive system. These pains can range from mild to severe and may come and go.
Nausea and regurgitation: These are less common symptoms but in certain cases, aerophagia can cause feelings of nausea and regurgitation or diarrhea and decreased appetite as a result of gas irritating or inflaming the digestive system
Difficulty swallowing: While not as common, aerophagia can sometimes result in difficulty swallowing, known as dysphagia. If you experience persistent trouble when swallowing, it's crucial to seek medical attention.
Aerophagia with CPAP: preventing symptoms
If you are using a CPAP machine to treat sleep apnea, you may experience symptoms of Aerophagia during the course of your treatment. Consult with your medical practitioner if you suspect that you are suffering from this condition. Here are some ways CPAP users can treat or prevent aerophagia while using a CPAP machine.
Proper Mask Fit: Ensuring the proper fit of your CPAP mask is essential in preventing aerophagia. A poorly fitting mask can result in air leakage, which may lead to increased swallowing of air. Work closely with your healthcare provider or CPAP supplier to find the right mask size and style that provides a secure seal without causing pressure points or discomfort. Regularly checking and adjusting the mask fit can help maintain an effective therapy while minimizing the risk of aerophagia.
Ramp Feature: Many CPAP devices offer a ramp feature that allows users to gradually increase the pressure over a set period. Utilizing this feature can help your body acclimate to the airflow and reduce the likelihood of aerophagia. Start with a lower pressure setting and gradually increase it until reaching the prescribed level. This gentle adjustment can give your body time to adapt, reducing the chances of excessive air swallowing.
Humidification: Dry air from CPAP therapy can sometimes contribute to aerophagia. Adding a heated humidifier to your CPAP system can help moisturize the air, reducing dryness and potential discomfort. The humidification feature helps keep your nasal passages and throat moist, minimizing the need for excessive swallowing of air. Consult with your healthcare provider or CPAP supplier to determine the appropriate level of humidification for your needs.
Positioning and Elevation: Sleeping in an elevated position can help prevent aerophagia during CPAP therapy. Elevating the head of your bed or using additional pillows to prop yourself up can aid in keeping the airway open and reducing the likelihood of excessive air swallowing. Additionally, sleeping on your side instead of your back can also promote better airflow and minimize the risk of aerophagia. Experiment with different sleeping positions and elevation techniques to find what works best for you.
Is CPAP Aerophagia Dangerous?
CPAP aerophagia, while uncomfortable and bothersome, is generally considered a harmless condition. It is important to note that aerophagia itself is not inherently dangerous. The excessive swallowing of air caused by CPAP therapy can lead to symptoms such as bloating, belching, and gas in the gastrointestinal system. However, it is essential to distinguish between aerophagia and potential complications that can arise from other medical conditions or underlying gastrointestinal disorders. If you experience persistent or severe symptoms, it is advisable to consult with your healthcare provider to rule out any other underlying issues. By working closely with your medical practitioner and implementing strategies to manage and prevent aerophagia, you can minimize its impact on your overall CPAP therapy experience and ensure effective treatment for sleep apnea.
Aerophagia causes
This condition can be caused by both physiological, psychological, and medical factors. For example, the way a person eats can cause too much air to be taken in, as can medical devices such as CPAP machines. People suffering from anxiety may inhale too much air during a panic attack, resulting in an increase in aerophagia symptoms. Understanding the underlying causes of aerophagia is key to managing and treating the condition effectively.
Physical Causes of Aerophagia
Eating habits: Rapidly consuming food or drink, chewing gum, or drinking carbonated beverages can increase the likelihood of swallowing air. These habits can introduce excess air into the digestive system, leading to aerophagia. Smoking is also a root cause and cutting it out should be considered if you are suffering from aerophagia.
Dentures: Ill-fitting dentures or the use of oral devices, such as dental braces or bite plates, can interfere with natural swallowing mechanisms, leading to increased air intake and aerophagia.
Mental Causes of Aerophagia
Anxiety and stress: Emotional factors such as anxiety and stress can contribute to aerophagia. During periods of heightened tension, individuals may unknowingly swallow air as a coping mechanism, exacerbating the condition.
Medical causes of aerophagia
Respiratory conditions: Certain respiratory conditions, such as chronic obstructive pulmonary disease (COPD) and asthma, can cause aerophagia. The altered breathing patterns associated with these conditions can result in the unintentional swallowing of air.
Gastrointestinal disorders: Various gastrointestinal disorders, including gastroesophageal reflux disease (GERD), irritable bowel syndrome (IBS), and gastroparesis, can be associated with aerophagia. These conditions can disrupt the normal functioning of the digestive system, causing excessive air swallowing.
Aerophagia treatment
There is no specific test to discern aerophagia, as it’s interlinked with other existing conditions. However, your medical practitioner may ask a series of questions about your medical conditions and lifestyle or habits to discern the presence of aerophagia.
Managing or treating this condition depends on the underlying causes and symptoms that any one person presents with. Treatment options may include:
Behavioral and dietary modifications: Making changes to your eating habits and lifestyle can significantly reduce aerophagia symptoms. It's advisable to eat slowly, chew food thoroughly, and avoid carbonated beverages. Additionally, managing stress through relaxation techniques, such as deep breathing exercises or meditation, can be beneficial.
Medications: In certain cases, your healthcare provider may prescribe medications to help manage aerophagia symptoms. For example, antacids or proton pump inhibitors (PPIs) may be recommended to reduce acid reflux and related symptoms. Prokinetic drugs can help regulate the movement of the digestive system and minimize the occurrence of aerophagia.
Dental adjustments: If ill-fitting dentures or oral devices are contributing to aerophagia, consulting with your dentist is crucial. They can make necessary adjustments or recommend alternative options to ensure proper fit and minimize air swallowing.
Treating underlying conditions: If aerophagia is secondary to an underlying medical condition, treating the root cause can help alleviate the symptoms. Working closely with your healthcare provider to manage conditions such as GERD, IBS, or respiratory disorders can have a positive impact on aerophagia.
Cognitive-behavioral therapy (CBT): CBT is a form of therapy that focuses on identifying and modifying negative thought patterns and behaviors. It can help address any psychological factors contributing to aerophagia, such as anxiety or stress. A trained therapist can guide you through CBT techniques to manage these underlying issues effectively.
Supportive measures: Alongside medical interventions, there are supportive measures you can take to manage aerophagia. These include practicing good posture, avoiding tight-fitting clothing around the abdomen, and refraining from smoking, as it can worsen symptoms.
Aerophagia relief
By implementing these preventive measures, individuals undergoing CPAP therapy can minimize the occurrence of aerophagia and ensure a more comfortable sleep apnea treatment experience. Remember to communicate any concerns or discomfort with your healthcare provider, as they can provide further guidance and adjustments to optimize your CPAP therapy.
It's important to note that while these tips can help prevent aerophagia during CPAP therapy, individual experiences may vary. It's essential to consult with your healthcare provider or sleep specialist for personalized recommendations and to address any specific concerns you may have.
Remember, maintaining consistent and effective CPAP therapy is vital for managing sleep apnea, so don't hesitate to seek support and guidance to ensure a successful treatment journey.
FAQs (Frequently Asked Questions)
What is aerophagia, and how is it related to CPAP therapy for sleep apnea?Aerophagia is a condition characterized by excessive swallowing of air, leading to symptoms such as bloating, belching, and gas in the gastrointestinal system. It can be related to CPAP therapy for sleep apnea because the constant air pressure from the CPAP machine can cause increased air intake, exacerbating aerophagia symptoms.
What are the common symptoms of aerophagia, and how can they be distinguished from other gastrointestinal disorders?
Common symptoms of aerophagia include frequent belching, abdominal bloating, flatulence, abdominal pain or cramps, and in some cases, nausea and regurgitation. These symptoms can overlap with other gastrointestinal disorders like GERD and IBS, making it challenging to distinguish aerophagia. However, excessive belching and the presence of air swallowing during CPAP therapy can be key indicators of aerophagia.
How can aerophagia be treated? Are there any medications or behavioral modifications that can help alleviate symptoms?
The treatment of aerophagia depends on the underlying causes and symptoms. Behavioral and dietary modifications such as eating slowly, chewing food thoroughly, avoiding carbonated beverages, and managing stress can significantly reduce symptoms. Medications like antacids or proton pump inhibitors (PPIs) may be prescribed to reduce acid reflux. Dental adjustments and treating underlying medical conditions can also help alleviate aerophagia symptoms. Cognitive-behavioral therapy (CBT) can be beneficial for addressing psychological factors contributing to aerophagia.
For individuals using CPAP machines, what are some specific measures they can take to prevent or manage aerophagia during therapy?
CPAP users can take several measures to prevent or manage aerophagia. Ensuring a proper mask fit is crucial to prevent air leakage and excessive swallowing of air. The ramp feature of CPAP devices allows gradual pressure increase, helping the body acclimate to airflow and reducing the likelihood of aerophagia. Adding a heated humidifier to the CPAP system can moisturize the air and reduce dryness. Sleeping in an elevated position and on the side can promote better airflow and minimize the risk of aerophagia. Consulting with healthcare providers or sleep specialists can provide personalized recommendations for optimizing CPAP therapy and managing aerophagia.
How do you stop aerophagia?
To stop aerophagia, various approaches can be taken. Behavioral modifications such as eating slowly, chewing food thoroughly, and avoiding carbonated beverages can help reduce air swallowing. Managing stress through relaxation techniques and seeking therapy for underlying psychological factors can also be beneficial. Additionally, ensuring a proper mask fit for CPAP users, utilizing the ramp feature, adding humidification, and adjusting sleeping positions can help prevent aerophagia during therapy.
When is aerophagia serious?
Aerophagia is generally not considered a serious condition on its own. However, it is essential to differentiate between aerophagia and potential complications arising from other medical conditions or underlying gastrointestinal disorders. If you experience persistent or severe symptoms, it is advisable to consult with your healthcare provider to rule out any underlying issues and determine appropriate management strategies.
As a leading supplier of durable and home medical equipment (DME and HME), ApriaHome sources and distributes a wide range of treatment solutions, including assistive respiratory equipment and monitoring solutions.
We're here to support you as you work toward your improved health and well-being. We strive to meet your ever-evolving healthcare requirements with individualized attention and premium quality treatment solutions.
Looking to add respiratory supplies? Browse our premium solutions and let us help you get the most out of every day.
Looking for advice? Our helpful agents are on call at (800) 780-1508 between 8:00 am - 10:00 pm EST daily. Get in touch today.





