Asthma and COPD share some similarities, such as shortness of breath, wheezing, and coughing. However, there are also some differences between the two conditions. Asthma symptoms are usually intermittent and can be triggered by allergens, exercise, or stress. COPD symptoms, on the other hand, are usually persistent and worsen over time.
In this article, we will discuss the similarities and differences between these two conditions, treatment options, and more.
What is Asthma?
Asthma is a chronic respiratory disease that affects the airways in the lungs. It causes inflammation and narrowing of the airways, making it difficult to breathe. Common symptoms of asthma include wheezing, shortness of breath, chest tightness, and coughing. Asthma can be triggered by various factors, such as allergens, infections, exercise, or stress. It can't be cured, but its symptoms can be controlled with medication and treatment.
What is COPD?
Chronic Obstructive Pulmonary Disease (COPD) is a long-term inflammatory condition of the lungs that results in blocked airflow. It's usually triggered by prolonged exposure to harmful irritants, predominantly cigarette smoke. Individuals with COPD have a heightened risk of developing heart disease, lung cancer, and other health issues. COPD symptoms encompass difficulty in breathing, coughing, production of mucus (sputum), and wheezing. These symptoms of COPD typically don't manifest until substantial lung damage has taken place, and they generally deteriorate over time, especially if exposure to smoking persists.
Asthma and COPD overlap
According to a study, as many as 50% of older people with obstructive airway disease may have overlapping diagnoses of Asthma and COPD. Another study found that 17% to 19% of patients with obstructive airway diseases had more than one condition or overlap. Overlap syndrome is recognized by the coexistence of increased variability of airflow in a patient with incompletely reversible airway obstruction. Patients typically have inflammatory features that resemble COPD.
While it is possible to have both Asthma and COPD, it is important to note that most people with Asthma will not develop COPD, and many people with COPD don’t have Asthma.
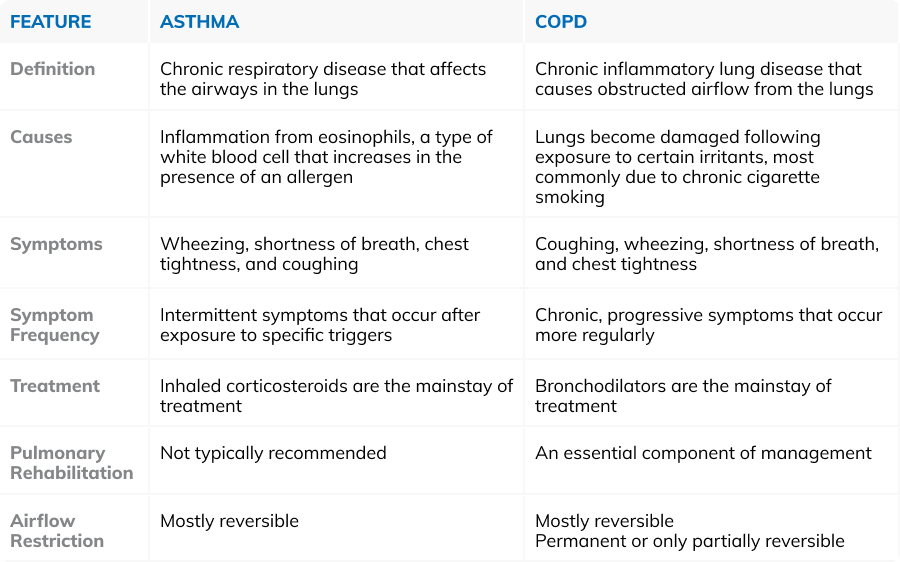
Here is a summary of the difference between COPD and Asthma (table):
Diagnosing Asthma and COPD
Diagnosing Asthma and COPD involves a combination of medical history, physical examination, and diagnostic tests. For Asthma, a doctor may conduct some tests to confirm the diagnosis and to exclude other lung conditions. These tests may include spirometry, peak flow measurement, and chest X-rays.
For COPD, tests may include lung function tests, chest X-rays, CT scans, arterial blood gas analysis, and laboratory tests.
If you suspect you have Asthma or COPD, it’s important to see a doctor for proper diagnosis and treatment.
Treatments for Asthma and COPD
The treatment for Asthma and COPD depends on the severity of the condition. Medications such as bronchodilators, inhaled steroids, and combination inhalers are commonly used to manage the symptoms of both Asthma and COPD. Pulmonary rehabilitation, healthy eating, and nutrition education are also helpful in managing these conditions. However, there are some differences in the treatment of Asthma and COPD.
Inhaled corticosteroids are the mainstay of Asthma treatment, while bronchodilators are the mainstay of COPD treatment. Pulmonary rehabilitation is an essential component of COPD management but is typically not recommended for Asthma patients. In addition, people with Asthma may need to take their medication daily to prevent symptoms, while people with COPD may only need to take medication when they experience symptoms.
COPD Medications
COPD is treatable, but it can’t be cured. Treatment aims at managing the condition and delaying progression through medication, physical therapy, and in severe cases surgery. Medications such as bronchodilators, inhaled steroids, and combination inhalers are commonly used to manage the symptoms of COPD.
Pulmonary rehabilitation is a program that includes exercise, breathing techniques, and education to help people with COPD improve their lung function and overall health. A healthy diet and nutrition education can help reduce inflammation in the body and improve lung function.
How to treat asthma
The treatment for asthma depends on the severity of the condition. Medications such as bronchodilators, inhaled steroids, and combination inhalers are commonly used to manage the symptoms of asthma.
Bronchodilators are medications that help relax the muscles around the airways, making it easier to breathe. Inhaled steroids help reduce inflammation in the airways, making them less sensitive to triggers. Combination inhalers contain both bronchodilators and steroids.
Coping with respiratory illness
Coping with respiratory illness can be challenging, but there are ways to manage the condition and live a fulfilling life. Here are some tips for coping with respiratory illness:
- Quit smoking and avoid secondhand smoke
- Take your medications as prescribed
- Follow a healthy diet and exercise regularly
- Avoid exposure to irritants such as air pollution, dust, and chemicals
- Get vaccinated against flu and pneumonia
- Manage stress and anxiety
- Join a support group
In addition, there are many resources available to help people with respiratory illness cope with their condition. Support groups, counseling, and pulmonary rehabilitation programs can all help manage the emotional and physical aspects of respiratory illness. It’s important to work closely with your healthcare provider to develop a treatment plan that works best for you.
The difference between Asthma and COPD
Understanding the differences between Asthma and Chronic Obstructive Pulmonary Disease (COPD) is crucial for effective management and treatment of these respiratory conditions. While both diseases share symptoms such as wheezing, coughing, and shortness of breath, their causes, progression, and treatment strategies significantly differ.
FAQs
Can Asthma turn into COPD?
Yes, people with Asthma can develop COPD later in life. A study found that as many as 50% of older people with obstructive airway disease may have overlapping diagnoses of Asthma and COPD ¹.
Can you have COPD and asthma together?
Yes, it is possible to have both Asthma and COPD. This is called Asthma-COPD Overlap Syndrome (ACOS).
What is the life expectancy of a person with COPD?
The life expectancy of a person with COPD depends on the severity of the disease, the age of initial diagnosis, and whether the person continues to smoke. The five-year life expectancy for people with COPD ranges from 40% to 70%, depending on disease severity.
What is the end stage of COPD?
End-stage COPD refers to the final stages of the disease. At this stage, you can expect to experience significant shortness of breath even when resting. Because of the degree of lung damage at this stage, you are at high risk for lung infections and respiratory failure.
As a leading supplier of durable and home medical equipment (DME and HME), ApriaHome sources and distributes a wide range of treatment solutions, including assistive respiratory equipment and monitoring solutions.
We're here to support you as you work toward your improved health and well-being. We strive to meet your ever-evolving healthcare requirements with individualized attention and premium quality treatment solutions.
Looking to add respiratory supplies? Browse our premium solutions and let us help you get the most out of every day.





