Living with diabetes, whether it's type 1 or type 2, can be challenging. Constant monitoring of blood sugar levels, insulin injections, and dietary restrictions can be overwhelming.
If you have diabetes, especially type 1 diabetes, you may need to take insulin to control your blood glucose levels. Insulin is a hormone that helps your body use glucose for energy. However, injecting insulin multiple times a day can be inconvenient, painful, and unpredictable. That's why some people with diabetes choose to use an insulin pump instead.
What Are Insulin Pumps?
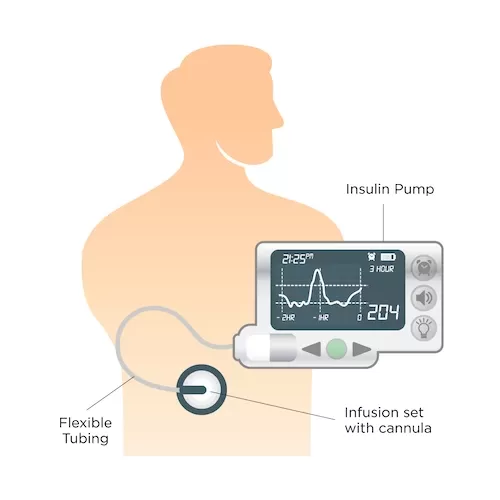
An insulin pump is a small device that provides continuous subcutaneous delivery of insulin through a tube and a needle or a patch that attaches to your skin. It can provide more flexibility, convenience, and accuracy than injections. It can also help you avoid low or high blood glucose levels, which can cause serious complications.
Unlike traditional insulin injections, which require multiple shots daily, insulin pump therapy offers a more precise and convenient way to manage diabetes. These pumps are typically about the size of a deck of cards and can be worn on a belt or carried in a pocket.
How Do Insulin Pumps Work?
Insulin pumps work by providing a steady stream of insulin into your body via a tiny tube called a cannula. This cannula is inserted just under your skin and can stay in place for several days. The pump itself is programmed to deliver a basal rate of insulin continuously, mimicking the natural release of insulin by a healthy pancreas. Additionally, you can use the pump to deliver extra insulin, known as a bolus, to cover meals or correct high blood sugar levels.
Benefits of Using Insulin Pumps
- Better Blood Sugar Control: Insulin pumps offer precise insulin delivery, which helps in maintaining stable blood sugar levels. This is crucial for both type 1 and type 2 diabetes patients.
- Flexibility: With insulin pumps, you have the freedom to adjust your insulin doses according to your lifestyle and changing needs
- Fewer Injections: Say goodbye to multiple daily injections. Insulin pumps require only one cannula insertion every few days.
- Improved Quality of Life: Many users report a significant improvement in their quality of life due to the convenience and ease of insulin pump use.
What are the pros and cons of using an insulin pump?
Using an insulin pump has many advantages over injections, such as:
- You only need to change the infusion site every three to four days, instead of injecting yourself several times a day.
- You can adjust the amount and timing of insulin delivery according to your needs, such as when you eat, exercise, or sleep.
- You can use only short or rapid-acting insulin, which reduces the variability and peaks of insulin action.
- You can program different basal rates (background insulin) for different times of the day or night, or use temporary basal rates for special situations.
- You can use bolus calculators (mealtime insulin) that help you determine how much insulin to take based on your blood glucose level, carbohydrate intake, and insulin sensitivity.
- You can monitor your blood glucose levels and insulin delivery with a continuous glucose monitor (CGM) that connects to your pump, if available.
- You can improve your quality of life, satisfaction, and glycemic control.
However, there can be a few drawbacks to making use of an insulin pump. These disadvantages of insulin pumps can include:
- You need to wear the pump all the time, except when bathing or swimming (depending on the model).
- You need to check your blood glucose levels frequently and calibrate your CGM if you use one.
- You need to learn how to use the pump correctly and troubleshoot any problems that may arise.
- You need to have a backup plan in case of pump failure, battery depletion, infusion site infection, or tubing occlusion.
- You need to pay for the pump and its supplies, which can be expensive and may not be covered by your insurance.
Who Can Benefit from Insulin Pumps?
Type 1 Diabetics
Insulin pumps are often considered the gold standard for managing type 1 diabetes. The ability to finetune insulin delivery to match daily activities and meals can be a game-changer for those with this autoimmune condition.
Type 2 Diabetes
While insulin pumps are not as commonly used for type 2 diabetes, they can still be highly effective in certain situations. People with type 2 diabetes who struggle to control their blood sugar with oral medications or traditional injections may find pumps to be a valuable addition to their treatment plan.
How to Get Started with an Insulin Pump
Getting started with an insulin pump involves several steps:
- Consultation with Your Healthcare Provider: Discuss your interest in using an insulin pump with your healthcare team. They will help determine if it's the right option for you.
- Choosing the Right Pump: There are various insulin pumps available, each with its unique features. Your healthcare provider will help you select the one that best suits your needs.
- Learning to Use the Pump: Once you have your pump, you'll receive training on how to use it properly, including how to insert the cannula and program the device.
- Continuous Monitoring: Regularly monitor your blood sugar levels to ensure the pump is effectively managing your diabetes. Adjustments may be needed over time.
How Insulin Pumps Work and How to Use Them
An insulin pump consists of three main parts:
- A reservoir or cartridge that holds the insulin
- A tubing system that connects the reservoir to the infusion site
- An infusion set that delivers the insulin into your body through a needle or a cannula
The pump also has a microcomputer that allows you to program the pump settings and control the delivery of insulin. Some pumps have buttons or touchscreens on the device itself, while others have remote controllers or smartphone apps.
To use an insulin pump, you need to:
- Fill the reservoir with short or rapid-acting insulin (such as Novorapid, Humalog, or Apidra) and attach it to the tubing system
- Insert the infusion set into a clean and dry area of your skin (such as your abdomen, buttocks, thighs, or arms) and secure it with tape or adhesive
- Program the pump with your settings, such as basal rates, bolus ratios, target blood glucose levels, and correction factors
- Deliver a bolus dose of insulin before each meal or snack by entering your blood glucose level and carbohydrate intake into the pump or using a bolus calculator
- Deliver a correction dose of insulin if your blood glucose level is too high or too low by entering your current blood glucose level into the pump
- Check your blood glucose levels at least four times a day and adjust your pump settings accordingly
- Change the infusion site every three to four days or sooner if it becomes red, swollen, painful, or infected
- Change the reservoir and tubing every two to three days or when they run out of insulin
- Replace the batteries when they are low or dead
Types of Insulin Pumps and How to Choose One
There are many types of insulin pumps available on the market. They vary in size, shape, features, functions, and prices. Some of the most common types are:
Traditional insulin pumps
These are pumps that have a reservoir and tubing system that connect to an infusion set. They are usually worn on a belt, in a pocket, or under clothing. They have buttons or touchscreens on the device itself or a remote controller that allows you to program and control the pump.
Tubeless insulin pumps
These are pumps that do not have tubing systems but attach directly to your skin with an adhesive patch. They are usually worn on your abdomen, arm, or leg. They have buttons or touchscreens on the device itself or a remote controller that allows you to program and control the pump.
Portable insulin pumps
These are pumps that are small and lightweight and can be carried in your hand, pocket, or purse. They have buttons or touchscreens on the device itself or a remote controller that allows you to program and control the pump.
To choose an insulin pump, you need to consider several factors, such as:
- Your personal preferences, lifestyle, and goals
- Your insurance coverage, budget, and warranty
- Your medical history, diabetes management, and complications
- Your doctor's recommendations, prescriptions, and training
- The pump's features, functions, and compatibility
- The pump's reliability, safety, and customer service
You should compare different models and brands of insulin pumps and consult with your doctor, diabetes educator, or pump specialist before making a decision.
Who should use an insulin pump?
Insulin pumps offer a promising solution for individuals living with both type 1 and type 2 diabetes. They provide better blood sugar control, greater flexibility, and a significant improvement in quality of life. If you're struggling to manage your diabetes with traditional methods, consider discussing insulin pumps with your healthcare provider. With the right guidance and support, you can embrace this innovative technology and take a significant step towards a healthier and more manageable life with diabetes.
FAQs about Insulin Pumps
Are insulin pumps painful to use?
The insertion of the cannula is relatively painless, and most users report minimal discomfort during daily use.
Can I swim or shower with an insulin pump?
Yes, most insulin pumps are waterproof and designed to be worn during activities like swimming and showering.
What if my pump malfunctions?
Manufacturers provide support and warranties for their pumps. Contact customer service for assistance in case of malfunctions.
Are insulin pumps covered by insurance?
Many insurance plans do cover insulin pumps, but it's essential to check with your provider for specific details.
As a leading supplier of durable and home medical equipment (DME and HME), ApriaHome sources and distributes a wide range of treatment solutions, including assistive diabetic equipment and monitoring solutions.
We're here to support you as you work toward your improved health and well-being. We strive to meet your ever-evolving healthcare requirements with individualized attention and premium quality treatment solutions.
Looking to add diabetic supplies? Browse our premium solutions and let us help you get the most out of every day.
Looking for advice? Our helpful agents are on call at (800) 7801508 between 8:00 am and 10:00 pm EST daily. Get in touch today.





