If you have chronic obstructive pulmonary disease (COPD), you may be wondering whether a nebulizer or an inhaler is the best way to deliver your medication. Both devices are used to treat respiratory conditions, but they have some differences that may affect your choice. In this article, we will explain what nebulizers and inhalers are, how they work, and what are the pros and cons of each one.
What is COPD?
COPD is a common lung disease that causes breathing difficulties, coughing, wheezing, and chest tightness. It is usually caused by long-term exposure to irritants such as cigarette smoke, air pollution, or occupational dust and chemicals. COPD is not curable, but it can be managed with medication and lifestyle changes.
One of the main goals of COPD treatment is to reduce inflammation and open the airways, which improves airflow and oxygen delivery to the lungs. This can help relieve symptoms and prevent complications such as infections, exacerbations, or respiratory failure. There are different types of medications that can achieve this goal, such as bronchodilators, corticosteroids, or mucolytics.
However, these medications need to reach the lungs to work effectively. This is where nebulizers or inhalers come in. These devices are designed to deliver medication in the form of a mist or a spray that can be inhaled into the lungs. Depending on the device, the medication can be pre-mixed or added by the user.
What is a Nebulizer?
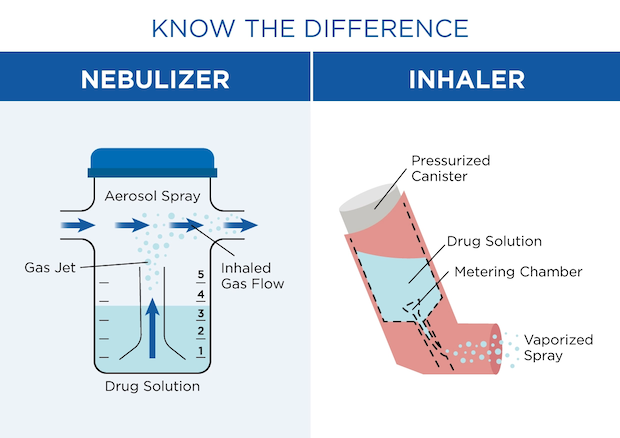
A nebulizer is a device that converts liquid medication into a fine mist that can be breathed in through a mouthpiece or a nebulizer mask. A nebulizer consists of a compressor, a tubing, and a cup that holds the medication. The compressor pumps air through the tubing and into the cup, which creates a mist that travels through the mouthpiece or mask to the lungs.
Nebulizers are usually used at home or in a hospital setting. They can deliver high doses of medication over a longer period, usually 10 to 15 minutes per session. The difference between a nebulizer and inhaler is that a nebulizer can also deliver multiple medications at once, which can be convenient for people who need more than one type of medication.
Benefits of using a Nebulizer
- Effective Medication Delivery: Nebulizers deliver a consistent and measured dose, ensuring that the medication reaches the lungs optimally.
- Suitable for All Ages: Nebulizers are suitable for children, the elderly, and anyone with limited hand coordination.
- Versatile Medication Options: Various COPD medications can be used in nebulizers, offering flexibility in treatment.
What is an Inhaler?
An inhaler is a handheld device that delivers medication in the form of a pressurized spray that can be inhaled into the lungs. An inhaler consists of a canister that contains the medication and a mouthpiece that releases the spray when pressed. There are different types of inhalers, such as metered-dose inhalers (MDIs), dry powder inhalers (DPIs), or soft mist inhalers (SMIs).
Inhalers are usually used on the go or as needed. They can deliver lower doses of medication over a shorter period, usually one or two puffs per session. Inhalers can only deliver one medication at a time, which means that people who need more than one type of medication may need to use more than one inhaler. This is one of the advantages of nebulizers over inhalers, which can disperse more than one medication at a time.
Benefits Of Using An Inhaler
- Portability: Inhalers can be carried in your pocket or purse, allowing you to take your medication wherever you go.
- Quick Action: Inhalers offer rapid relief, making them ideal for acute COPD symptoms.
- No Power Source Required: Unlike nebulizers, inhalers do not require electricity, making them more versatile in various settings.
Nebulizer versus Inhaler
Both nebulizers and inhalers have advantages and disadvantages that may influence your decision. Here are some of the main factors to consider:
- Effectiveness: Both devices are effective in delivering medication to the lungs, but some studies suggest that nebulizers may be more effective in certain situations, such as during exacerbations or for people with severe COPD. However, this may depend on individual factors such as lung function, technique, or preference.
- Convenience: Inhalers are more convenient than nebulizers because they are portable, easy to use, and require less maintenance. Nebulizers are bulkier, require electricity or batteries, and need to be cleaned regularly. Inhalers are also faster than nebulizers because they take less time to administer the medication.
- Cost: Nebulizers are more expensive than inhalers because they require more equipment and supplies. Nebulizers also need a prescription from a doctor, while some inhalers can be bought over the counter. However, some insurance plans may cover part or all of the cost of nebulizers or inhalers.
- Side effects: Both devices can cause side effects such as coughing, throat irritation, or mouth dryness. However, nebulizers may cause fewer side effects than inhalers because they deliver smaller particles that are less likely to irritate the airways. Nebulizers may also reduce the risk of oral thrush or hoarseness caused by corticosteroids.
Which is better, an inhaler or nebulizer?
When making these kinds of decisions, it’s always crucial to consult with your healthcare practitioner first. There are several reasons why an inhaler or nebulizer might better suit your requirements. Here are some factors to consider when making this decision:
- Severity of COPD: Nebulizers are often recommended for severe COPD cases, while inhalers may suffice for milder forms of the disease.
- Personal Preference: Some individuals prefer the convenience of inhalers, while others may find nebulizers more comfortable to use.
- Mobility and Lifestyle: Your daily activities and mobility should also influence your choice. Inhalers are better suited for those with an active lifestyle.
For COPD a nebulizer or inhaler are both effective devices that can help you manage your condition and improve your breathing. However, they have different features that may suit different people better. You should weigh the pros and cons of each device and consult your doctor before choosing one. You should also follow the instructions on how to use, clean, and store your device properly to ensure your device continues to work well for you.
FAQs
Can I use both an inhaler and a nebulizer?
Yes, you can use both devices depending on your needs and preferences. Some people may use a nebulizer at home and an inhaler when they are out. Some people may use a nebulizer for maintenance therapy and an inhaler for rescue therapy. Some people may use a combination of both devices for optimal results. However, you should always consult your doctor before using any device or medication.
How often should I use a nebulizer or an inhaler?
The frequency of using a nebulizer or an inhaler depends on your condition, symptoms, and treatment plan. Your doctor will prescribe the best schedule for you based on your needs and goals. Generally, nebulizers are used once or twice a day for maintenance therapy, while inhalers are used as needed for rescue therapy or before exercise. However, this may vary depending on the type and dose of medication you are using.
How do I know if my nebulizer or inhaler is working?
You can tell if your nebulizer or inhaler is working by monitoring your symptoms, lung function, and quality of life. You should notice an improvement in your breathing, coughing, wheezing, chest tightness, or exercise tolerance after using your device. You should also check your peak flow meter or spirometer regularly to measure how well your lungs are working. You should also keep track of how often you use your device and how much medication you need. If you notice any worsening of your symptoms, lung function, or quality of life, you should contact your doctor as soon as possible.
As a leading supplier of durable and home medical equipment (DME and HME), ApriaHome sources and distributes a wide range of treatment solutions, including assistive respiratory equipment and monitoring solutions.
We're here to support you as you work toward your improved health and well-being. We strive to meet your ever-evolving healthcare requirements with individualized attention and premium quality treatment solutions.
Looking to add respiratory supplies? Browse our premium solutions and let us help you get the most out of every day.
Looking for advice? Our helpful agents are on call at (800) 780-1508 between 8:00 am - 10:00 pm EST daily. Get in touch today.





