Chronic Obstructive Pulmonary Disease (COPD) is a lung condition that makes breathing a daily challenge. With millions grappling with this ailment, understanding medication for COPD is crucial for managing symptoms and improving quality of life.
What is COPD?
COPD encompasses several respiratory diseases that make it hard to breathe. They are often progressive, meaning the condition can worsen over time. Living with COPD can feel like trying to breathe through a straw; it's frustrating and frightening. But here's the silver lining: with the right COPD medication and treatment strategies, many people manage their symptoms effectively and lead full, active lives.
The Role of Medication for COPD Treatment
Medications play a pivotal role in managing COPD. They help to reduce symptoms, prevent complications, and slow disease progression. But with a myriad of options, it's easy to get lost in a sea of inhalers, pills, and nebulizers. Let's clear the air with answers to some common questions about COPD medications.
What Are the Main Types of COPD Medications?
COPD medications come in various forms, each with a specific role in managing the disease.
-
Bronchodilators
These are the cornerstone of COPD treatment. They relax the muscles around your airways, making it easier to breathe. They come in short-acting forms for quick relief and long-acting forms for ongoing control.
-
Corticosteroids
These reduce inflammation in the airways, making them less likely to react to triggers. They're often combined with bronchodilators for a more powerful effect.
-
Phosphodiesterase-4 Inhibitors
A newer class of medication, these reduce inflammation and relax the airways to improve breathing.
-
Mucolytics
These help to thin the mucus in the airways, making it easier to cough up and clear out.
-
Antibiotics and Antivirals
These are used to treat infections, which can exacerbate COPD symptoms.
How Do I Know Which COPD Medication Is Right for Me?
The "best" COPD medication varies from person to person. It's a decision you'll make with your healthcare provider, based on:
- The severity of your COPD
- Your symptoms
- How well you tolerate the medication
- Your lifestyle and preferences
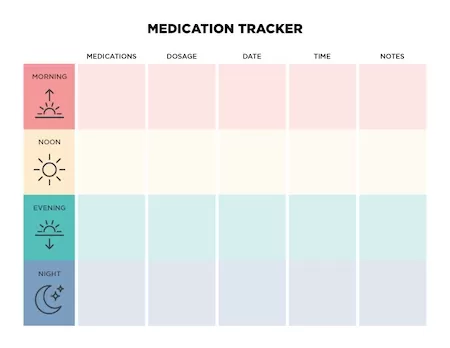
Keeping a chart can help you track your medications, dosages, and schedules. This ensures you're taking everything correctly and allows you to see what's working and what isn't when it comes to managing your COPD medication.
Here’s an example of a COPD medications chart that you can follow:
Can Lifestyle Changes Complement COPD Medication?
Absolutely! Quitting smoking, exercising, and following a healthy diet can all enhance the effectiveness of your COPD medication.
Lifestyle changes, including gradual and gentle exercise, can be a great way of improving your chronic condition. Gentle exercise done in consultation with your healthcare provider can help you strengthen your respiratory muscles, and ultimately improve your oxygen intake through increasing your heart rate and blood flow. Some gentle exercises to consider include swimming, walking, and yoga. Certain breathing exercises can also help you improve your lung capacity, we’ve put together this guide to breathing exercises for COPD sufferers.
Diet also plays an important role in managing chronic respiratory conditions. Foods that can exacerbate COPD include heavily spiced foods, fried food, and certain dairy products, while whole grains and leafy vegetables may ease discomfort. Read more about managing COPD through diet.
Can I Use Over-the-Counter Medications for COPD?
While there's no over-the-counter cure for COPD, certain OTC medications can help manage symptoms. Always consult with your doctor before adding any OTC meds to your regimen, as it’s never wise to mix different types of medications without knowing how your body will react. It’s always best to stick to the prescription medications provided by your doctor.
How Can I Manage COPD Exacerbations?
COPD exacerbations are sudden flare-ups of symptoms. They can be managed with a combination of fast-acting bronchodilators, corticosteroids, and sometimes antibiotics or antivirals.
In colder months you may find breathing harder. This can be due to both drier winter air and indoor heating. During summer, flare-ups may be a result of increased dust, pollen, or air pollution. It’s best to consider your environment carefully to manage COPD exacerbation.
Are there alternative treatments to traditional COPD medication?
The gold standard in COPD treatment are the medications listed above. However, there are other ways that you can alleviate symptoms of COPD.
These can include pulmonary rehabilitation, oxygen therapy, and lifestyle changes discussed earlier. However, always consult with your healthcare provider before exploring new avenues of treatment.
COPD Treatment to Improve Your Lifestyle
COPD medication is a lifeline for those with this chronic disease. Understanding your options, knowing how to manage them, and working closely with your healthcare provider are key to breathing easier. Remember, while COPD is currently incurable, with the right medication and lifestyle changes, you can maintain an active, fulfilling life.
Remember, this guide is a starting point. Always consult with your healthcare provider for advice tailored to your condition.
FAQs
Q: What is the best COPD medication?
The best medication is one that's tailored to your specific needs. It's often a combination of drugs that work together to manage symptoms.
Q: Are there natural remedies for COPD?
While natural remedies can support COPD treatment, they should never replace prescribed medications. Discuss any supplements or herbs with your doctor.
Q: How often will my COPD medication change?
It depends on how your COPD progresses and how well your current treatment is working. Regular check-ups are essential.
Q: Can I use a nebulizer for COPD medication?
Yes, nebulizers can be used to deliver medication directly to the lungs and are especially helpful for those who have difficulty using inhalers.
Q: Is it safe to take COPD medication during pregnancy?
Always consult with your doctor about medication use during pregnancy.
As a leading supplier of durable and home medical equipment (DME and HME), ApriaHome sources and distributes a wide range of treatment solutions, including assistive respiratory equipment and monitoring solutions.
We're here to support you as you work toward your improved health and well-being. We strive to meet your ever-evolving healthcare requirements with individualized attention and premium quality treatment solutions.
Looking to add respiratory supplies? Browse our premium solutions and let us help you get the most out of every day.
Looking for advice? Our helpful agents are on call at (800) 780-1508 between 8:00 am - 10:00 pm EST daily. Get in touch today.





