Living with COPD (Chronic Obstructive Pulmonary Disease) can be challenging, but incorporating exercises for COPD into your daily routine can significantly improve your quality of life. If you're unsure whether exercise is safe for you, which exercises are suitable, and how they can help manage COPD, this article is here to guide you through the process.
Understanding COPD and Exercise
What is COPD?
Chronic Obstructive Pulmonary Disease (COPD) is a progressive lung condition that obstructs airflow, making it difficult to breathe. It encompasses conditions like chronic bronchitis and emphysema, often caused by smoking or long-term exposure to air pollutants. If you have COPD, you may experience shortness of breath, wheezing, chest tightness, and a persistent cough.
These symptoms can make it hard to perform daily activities like walking, climbing stairs, or carrying groceries. They can also affect your mental health, causing anxiety, depression, or social isolation.
But there is hope. Exercising with COPD can help by strengthening your respiratory muscles, improving your oxygen use, and reducing your symptoms. Exercise can also improve your cardiovascular health, muscle strength, balance, flexibility, and mood.
Exercise cannot reverse lung damage, but it can change the way you feel, breathe, and function. It can help you stay active and independent and enjoy a better quality of life.
Can exercise make COPD worse?
Many COPD patients wonder if exercise is safe for them, given their respiratory condition. The answer is that exercise for COPD can be not only safe but also highly beneficial. Regular physical activity can improve lung function, increase muscle strength, enhance cardiovascular fitness, and elevate overall well-being. However, it's crucial to approach exercise with caution and follow specific guidelines.
COPD and Exercise Tolerance
It's essential to be mindful of your exercise tolerance when managing COPD and to take the correct COPD exercise precautions. Pay attention to any signs of fatigue, shortness of breath, or dizziness during physical activity. Always consult with your physician before taking on physical exercise. If you experience severe discomfort, stop exercising immediately and seek medical advice.
How Exercise Helps People with COPD
Exercise has many benefits for people with COPD. Here are some of them:
-
It strengthens your respiratory muscles.
The muscles that help you breathe, such as the diaphragm and the intercostal muscles (between the ribs), can become weak and inefficient due to COPD. Exercise can help them work better by increasing their endurance and power. This can make breathing easier and more comfortable. -
It improves your oxygen use.
Chronic Obstructive Pulmonary Disease can impair your ability to get enough oxygen into your blood and deliver it to your organs and tissues. Exercise can improve your oxygen uptake by increasing your heart rate and blood flow. It can also enhance your oxygen delivery by improving your hemoglobin levels (the protein that carries oxygen in red blood cells) and your capillary density (the number of tiny blood vessels that reach your muscles). -
It reduces your symptoms.
Exercise can help you reduce some of the common symptoms of COPD, such as coughing, wheezing, mucus production, and chest tightness. Exercise can also help you clear your airways by loosening the mucus and making it easier to cough up. This can prevent infections and complications like pneumonia. -
It improves your cardiovascular health.
This condition can increase your risk of developing heart disease and stroke due to the strain it puts on your heart and blood vessels. Exercise can lower this risk by improving your blood pressure, cholesterol levels, blood sugar levels, and inflammation markers. Exercise can also prevent or treat conditions like diabetes, obesity, and metabolic syndrome that are associated with COPD. -
It increases your muscle strength.
COPD can cause muscle wasting and weakness due to lack of physical activity, poor nutrition, inflammation, and steroid use. Exercise can prevent or reverse this by stimulating muscle growth and repair. Stronger muscles can help you perform daily tasks more easily and prevent falls and injuries. -
It enhances your balance and flexibility.
Lung disease can affect your balance and flexibility due to reduced mobility, muscle weakness, joint stiffness, or side effects of medications. Exercise can improve these aspects by increasing your range of motion, coordination, stability, and posture. Better balance and flexibility can help you prevent falls and injuries.
Exercises for COPD rehabilitation
Walking
Walking is an excellent low-impact exercise for COPD patients. Start with short distances and gradually increase your walking time as you build endurance. Consider walking indoors on a flat surface to avoid exposure to environmental triggers, such as cold air or pollution. Remember to maintain a steady pace and take breaks as needed.
Stationary Cycling
Slow stationary cycling is a safe and effective way to improve cardiovascular fitness without putting excessive strain on your lungs. You can adjust the resistance to a comfortable level and cycle at your own pace. This exercise engages various leg muscles and promotes overall circulation.
Strength Training
Strength training exercises that target major muscle groups can enhance your physical strength and make daily activities easier to perform. Utilize light weights or resistance bands and perform exercises such as leg curls, arm raises, and seated chest presses. Always breathe consistently during strength training and avoid holding your breath. Make sure you consult with a professional trainer before undertaking strength training to ensure you’re targeting the correct muscles and not damaging delicate tissue.
Yoga
Yoga can be beneficial for COPD patients as it combines gentle physical movements with breath control and relaxation techniques. Choose yoga poses that promote lung expansion and focus on controlled breathing throughout the practice. Remember to avoid positions that put pressure on your chest or make you feel uncomfortable.
Breathing Exercises for COPD
Diaphragmatic Breathing
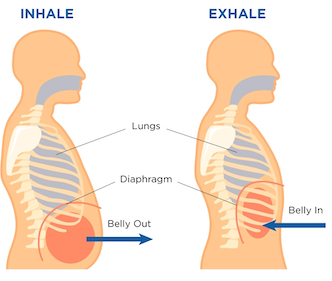
Diaphragmatic breathing, also known as deep breathing or abdominal breathing, is a simple yet effective exercise for COPD sufferers to strengthen the diaphragm and improve lung function. To perform this exercise, sit or lie down comfortably and inhale deeply through your nose, allowing your abdomen to expand fully. Exhale slowly through pursed lips, emptying your lungs completely. Repeat this for several minutes daily.
Pursed-Lip Breathing
Pursed-lip breathing is another valuable technique to ease shortness of breath and improve oxygen exchange. Inhale gently through your nose for two counts, then exhale through pursed lips for four counts. This exercise helps keep your airways open longer and reduces the work of breathing during physical activity.
Discover more breathing exercises for COPD.
Can COPD Be Reversed with Exercise?
Unfortunately, COPD is a chronic condition, and while exercise cannot reverse the damage to your lungs, it can significantly improve your symptoms and slow down disease progression. Regular physical activity helps optimize lung function, reduces breathlessness, and enhances your ability to perform daily tasks independently.
Incorporating exercise into your daily routine can be a game-changer for COPD patients. Not only does it improve lung function and overall fitness, but it also enhances your mental well-being and empowers you to manage COPD more effectively. Remember to consult with your healthcare provider before starting any exercise program, and always listen to your body's signals during physical activity. With dedication and the right approach, exercise can become an integral part of your COPD management plan, bringing you closer to a more active and fulfilling life.
FAQs
- Can exercise make COPD worse?
Exercise, when done correctly and within your limits, should not make COPD worse. However, it's crucial to consult with your healthcare provider before starting any exercise program to ensure it is safe and appropriate for your condition.
- How often should I exercise?
The frequency of exercise depends on your individual condition and fitness level. Start with short sessions and gradually increase them over time. Aim for at least 30 minutes of moderate exercise most days of the week.
- Can I do exercises other than the ones mentioned here?
Absolutely! While the exercises mentioned in this article are suitable for many COPD patients, you can explore other activities like swimming, tai chi, or gentle aerobics. Just remember to choose exercises that won't exacerbate your symptoms and always exercise in a safe environment.
As a leading supplier of durable and home medical equipment (DME and HME), ApriaHome sources and distributes a wide range of treatment solutions, including assistive respiratory equipment and monitoring solutions.
We're here to support you as you work toward your improved health and well-being. We strive to meet your ever-evolving healthcare requirements with individualized attention and premium quality treatment solutions.
Looking to add respiratory supplies? Browse our premium solutions and let us help you get the most out of every day.
Looking for advice? Our helpful agents are on call at (800) 780-1508 between 8:00 am - 10:00 pm EST daily. Get in touch today.





